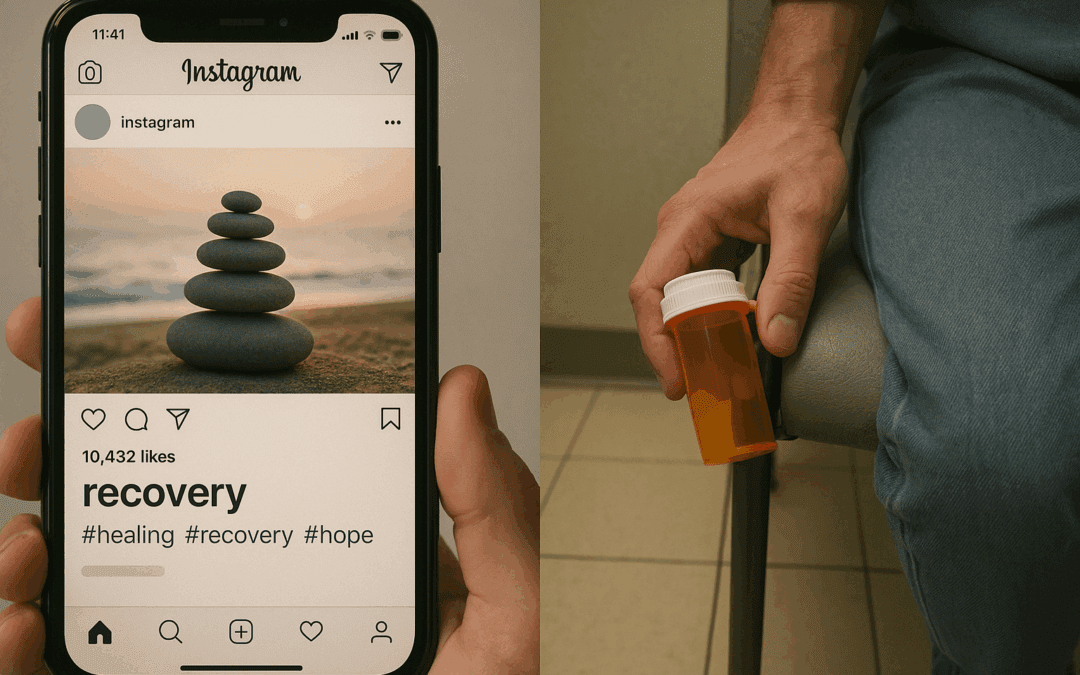
What if the very stories and guides designed to reach families in crisis feel flat, clinical, or even performative—leaving loved ones more adrift than before? Every September, digital feeds overflow with Recovery Month articles, yet precious few ring true for those pacing cold ER floors or staring at empty pill bottles. The gap between marketing and lived reality whispers an uncomfortable question: Who, exactly, are we writing for?
Recovery isn’t a hashtag. For families and clinicians, it’s a nightlight burning through sleepless uncertainty—a game of silent signals and unasked questions. Yet, too often, National Recovery Month content floats above real pain, layered in jargon and vague hope. You deserve a voice that meets that ache with candor, guidance, and dignity.
Key Takeaways
- Most Recovery Month content floats above real pain—families need candor, not hashtags.
- Clinical wisdom gets lost in translation; structured content bridges the gap between panic and plan.
- Trust emerges when programs acknowledge limits, protect privacy, and offer actionable next steps—not miracle stories.
- Content that merely fills calendars is noise; content that closes gaps is medicine.
Exhausted by hollow campaigns? Let Content Done Write build you trust-first, clinically vetted mental health content that matters. Contact us to save hours—and change lives.
Why Clinical-Led Content Wins (and What Usually Goes Wrong)
Content designed for National Recovery Month should do more than fill a social calendar; it should close the silent chasm between what families need and what practitioners can deliver without forsaking their own well-being. The trouble? Most behavioral health content is crafted in a parallel universe—a place where the raw tensions and private agonies of addiction and recovery are sanded down, abstracted, or worst of all, ignored.
Families show up needing clear, honest answers: What now? How bad is it, really? Who can help? They’re not looking for medical white papers, but neither are they helped by glib copy that hints at hope without a lifeline. Meanwhile, clinicians hold oceans of wisdom, but are bombarded by inboxes and protocols, left with little time to craft the words that might pull a family out of harm’s way. The result is a frustrating paradox: clinical supervision is absent from most content, jargon builds brick walls, and the ethics of telling patient stories become a minefield, risking trust at every turn. Too often, assets wind up orphaned—published, but never measured or iterated, untethered from the larger work of healing.
What this guide delivers is a simple, repeatable sprint: one any treatment program can deploy, whether with internal champions or with a seasoned mental health ghostwriter. The goal? Content that is accessible, evidence-aligned, and measurable—without draining precious clinical hours or compromising privacy.
Want content that sidesteps common pitfalls? Partner with Content Done Write to create family-first, review-ready resources—protecting your clinical time and your program’s reputation.
Further Reading:
Week 1 — The Cornerstone Family Guide
This is your digital hand extended to the weary, the worried, and the waiting. A cornerstone guide isn’t just information—it’s orientation. Imagine a resource that opens with empathy, makes no assumptions, and’s organized so a frantic parent or partner can find what they need quickly and safely. Here’s the blueprint:
Structure to Swipe
1. Empathy Lead-In
Begin by assuring the reader: “This guide takes about 10 minutes to read and will leave you knowing what steps can help next. You’re not expected to have the answers; that’s our job.”
2. The 7 FAQs—Each as a Section
Every family wants to know:
- What is happening right now—are we in crisis?
- What are our next steps, hour-by-hour?
- Who do we call, and when?
- How does insurance really work—for this?
- What level of care is right, and why?
- What does real recovery look like?
- How do we handle setbacks and relapses?
Every answer ends with a practical touchpoint: “What to ask your clinician.”
3. Visual Aids That Actually Help
- Level-of-Care Decision Tree: One glance, immediate clarity.
(see resource: ASAM Levels of Care Explained) - Insurance Readiness Checklist: Key questions to ask, pitfalls to avoid.
(reference: NAMI Insurance Basics) - Green Flags vs. Red Flags: Simple table distinguishing promising signs from warning signals when evaluating a program.
4. Trust Layers and Compliance
Include a clear clinician byline, date of last clinical review, and a “Crisis Box” with hotline contacts. Transparently cite decision points and underscore ethical boundaries—such as “Stories on this site have been changed to protect privacy.”
On-page SEO & Navigation (No Gimmicks):
- Clear meta title/description
- FAQ schema for search engines
- Breadcrumbs and links to in-depth program pages
- Last updated timestamp
Paste-ready CTA: “Download the Family Intake Checklist (PDF).”
Build family trust with accessible guides—work with Content Done Write for rapid, clinician-reviewed assets built for real-world need, not empty metrics.
Week 2 — Ethical Storybank (2–3 Vignettes, 300–500 words each)
Recovery is never a straight path; it’s made of stories that hush the bravado and amplify real hope. But every story told carries the responsibility to protect privacy—and never glorify the very harm we’re meant to help.
Protecting Consent & Privacy
Vignettes must only feature de-identified details; in some cases, combine stories or use composites to shield identities. Each narrative confirms written consent, with an explicit statement that unique attributes are altered to block trace-back. For more on privacy ethics, visit Substance Abuse and Mental Health Privacy.
Narrative Pattern to Use
Follow a heartbeat rhythm: “Moment of decision → Support received → Skill learned → What changed.” The effect? Narratives that neither romanticize nor reduce, but instead bear witness to the reality and resilience of recovery.
Clinical Sidebar
Each story includes a “Team Takeaway”—a sidebar that spotlights an evidence-laced lesson (e.g., the role of medication adherence, how CBT skills supported relapse prevention, what helped families re-engage). Whenever possible, link to research or consensus guidelines, such as CBT for Addiction.
Paste-ready CTA: “Ask a Clinician (48-hour response).”
Your program deserves ethically crafted stories that both uplift and protect—commission Content Done Write to expand your impact while maintaining privacy and trust.
Week 3 — 10-Minute Clinician Q&A (Video + Transcript)
Too often, direct clinical expertise gets lost in translation. A structured, easy-to-film Q&A video opens the door for prospective families seeking reliable guidance—and ensures your expert voice is always on call.
Run-of-Show: The Key Questions
Film and transcribe answers to eight core questions:
- What are the main levels of care, and who are each for?
- How do you handle dual diagnoses or co-occurring disorders?
- How do medications (including MAT) fit, and what are their limitations?
- What role do families play throughout treatment?
- What should we know about insurance, coverage, and cost?
- How can we recognize and intervene in a crisis?
- What happens after formal treatment ends?
- How should we approach setbacks or relapses?
Repurpose Map
- Skimmable post: Transcript with timestamps for each question.
- Clips: 60-90 second highlights for social outreach.
- Quote Cards: Pull impactful statements for graphics or email teasers.
- Email teaser: Send a digest to families and referral partners.
Accessibility Checklist
- Closed captions on video
- Transcript and alt text for visuals
- “Last reviewed” date on page
For more on accessible health content, see WebAIM: Accessibility in Video and Health Literacy Online.
Paste-ready CTA: “Tour Our Program (virtual session).”
Multiply your Q&A reach—book a strategy call with a mental health ghostwriter from Content Done Write to produce professional, HIPAA-ready content you can repurpose all year.
Week 4 — Build the Trust Hub (Your Always-On Front Door)
A Trust Hub isn’t a promotional afterthought—it’s the tip of the spear for your recovery program, always open, always honest.
Hub Tiles: Key Resources at a Glance
- Family Guide
- Stories
- Q&A
- Outcomes & Credentials
- Family Resources (support groups, hotlines, financial aid)
Proof Stack
Every claim is supported. Share staff bios with credentials and information about your supervision model. Detail the outcomes methodology. Prominently display the grievance/feedback pathway and your privacy and advertising policies.
Navigation
Keep your navigation human-friendly: breadcrumbs, related links, and a prominent “Start Here” banner guide families no matter where they land.
Explore examples and design inspiration at The Kennedy Forum’s Advocacy Toolkits.
Ready to be seen as the program families trust first? Let Content Done Write engineer your Trust Hub with clinical nuance and digital best practices.
What Great Looks Like vs. What to Avoid
What truly moves the needle is content that translates clinical nuance into plain language, armed with actionable questions for families and a clear-eyed account of where your program’s scope starts—and stops.
Great content allows for nuance, acknowledges uncertainty, and orients families without smoke or mirrors.
To Avoid at All Costs:
- Symptom checklists without context or disclaimers
- Testimonials that could expose identity
- PDFs that bury practical advice under mountains of jargon
- Automated or AI-generated assets that lack human review
For further standards, see Plain Language Guidelines
Measurement That Matters (Clinical + Operational)
Every word, every artifact, should track the metrics that spell authentic engagement—not vanity stats.
Trust & Clarity
- Time on page
- Scroll depth
- “Was this helpful?” instant polls
- Declines in repetitive intake questions
Access
- Calls and consults started after engaging with the hub
- Video Q&A plays
- Resource checklist downloads
Operational KPIs
- Review-cycle time, SME minutes spent
- Age of content since last clinical review
A simple dashboard, reviewed weekly, ensures your program iterates rather than guessing.
Explore sample metrics at Content Marketing Institute: Measurement Framework.
Commission Content Done Write to not just craft but help you measure content that delivers clarity, trust, and real access.
How to Work With a Mental Health Ghostwriter (So Your Team Gains Time, Not Tasks)
Outsourcing doesn’t mean abdicating control—it’s a shortcut to quality, if done well. Here’s how to make it work:
- The handoff: You provide key protocols and a subject matter expert; the ghostwriter does drafting, research, proper sourcing, and clinical schema—requiring as little as 90 minutes of your total time.
- The review rhythm: Approve in a single batch with tracked changes—no endless comment chains or Google-doc chaos.
- Attribution: Choose between personal clinician byline (“drafted in partnership with a medical writer”) or a program-level byline—each has pros and cons for credibility and brand vision.
- Quality: Set a high bar: expertise, ethical citations, crisis-routing links, and a regular refresh schedule.
Need consistent, compliant, and clinically sound patient-facing content? Let a mental health ghostwriter from Content Done Write shoulder the creative lift so your team can stay focused on care.
Frequently Asked Questions (for Clinical Directors)
How do we keep this HIPAA/42 CFR Part 2 safe?
Only publish de-identified case material with explicit, written patient consent or composites. Never disclose combinations of symptoms or outcomes unique enough to trace.
What if we don’t have outcomes data yet?
Focus on transparency: describe what you ARE measuring, your methodology, and plans for future reporting—even if the numbers are still coming.
How do we involve lived-experience voices ethically?
Invite patients and families to participate in consented, anonymous feedback. Pay attention to power dynamics and always privilege privacy over narrative drama.
What breaks trust with families—and how do we avoid it?
Breaking trust springs from exaggeration, omission, or “miracle story” tropes. Stick to candor about limits and what your program can and can’t do.
How do we adapt this sprint for specialty programs?
Tweak FAQ and decision-tree assets for unique needs (adolescents, dual-diagnosis, perinatal, etc.), and ensure lived-experience voices are reflected in ways safe for each population.
For more operational guidance, visit HIPAA Journal’s Content Publishing Guidelines.
Lead With Care, Publish With Rigor
Content that merely fills a calendar is noise; content that closes the gap between panic and plan is a balm. As National Recovery Month lights up the digital landscape, let your words lead with candor, care, and precision. Less noise, more clarity. Safer stories, stronger access. It’s not just better marketing—it’s better medicine.
You can have digital content that embodies clinical wisdom, protects time and privacy, and builds authentic trust—without exhausting your staff. Ready for content that helps families, clinicians, and your brand flourish? Contact Content Done Write today. I’m the mental health ghostwriter who can help you meet this September—and every month—with storytelling that truly makes a difference.

Recent Comments